Ground-Breaking Study on Treatment of U.S. War Veterans with TBI and PTSD Published on November 22, 2011 the long-awaited preliminary results of the LSU Pilot Trial of hyperbaric oxygen therapy in chronic blast-induced mild-moderate traumatic brain injury (TBI)/post-concussion syndrome (PCS) and post-traumatic stress disorder (PTSD) were published online. And, the results are stunning. The article appears in the prestigious peer-reviewed Journal of Neurotrauma as a Fast Track article under the Open Access Option at: liebertonline.com, and we now have it posted here on hbot.com! The study, originally designed to test safety and feasibility, reinforced the historical safety and feasibility of the protocol, but at the same time significantly improved the veterans, their disabling symptoms, and quality of life.
The study was conducted by Dr. Paul G. Harch and colleagues at LSU School of Medicine New Orleans, the University of North Dakota School of Medicine, and the University of California, Irvine, School of Medicine and Amen Clinics. Sixteen active duty and retired U.S. veterans were treated with hyperbaric oxygen therapy nearly three years after brain injuries and PTSD caused by improvised explosive device (IED) and rocket-propelled grenade explosions. All of the veterans had been diagnosed by military and/or civilian specialists with PCS and PTSD before coming to New Orleans to enter the study. These diagnoses were confirmed by the study authors before treatment. All veterans were significantly affected by a variety of classic PCS and PTSD symptoms and had abnormal neurological exams and cognitive testing.
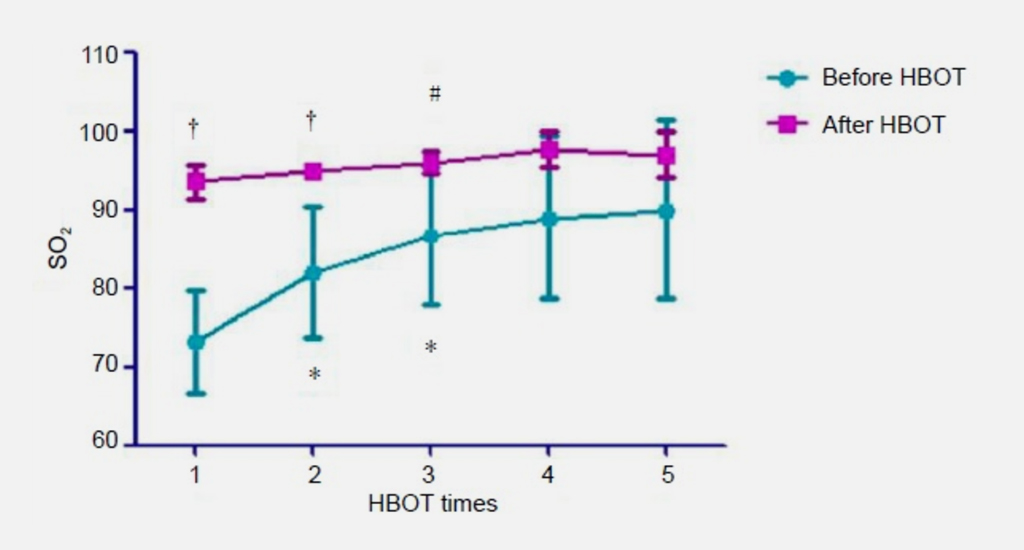
After forty low pressure hyperbaric oxygen treatments in one month the veterans achieved substantial improvements in symptoms, physical exams, cognitive testing, quality of life, and brain blood flow. The veterans achieved a nearly 15 point increase in IQ which is equivalent to the change from the average IQ of a clerical worker or construction worker to the IQ level of a college instructor or engineer. The magnitude of this increase, along with the significant improvements in short term memory, attention/concentration, and executive function was far greater than has been demonstrated in placebo controlled studies or in studies that documented improvements due to short-interval test/retest effects. These cognitive gains also strongly suggested the ability of these and similarly treated veterans to return to college level education or achieve higher salary employment.
The veterans also experienced a marked reduction in post-concussion symptoms, including headaches, the primary marker of blast-induced TBI, that was reflected in significant improvements in quality of life. Simultaneously, the veterans experienced an average 50% reduction in depression symptoms. Depression has been identified as one of the top veteran mental health afflictions in the Rand Report of 2008. Suicidal ideation was also significantly reduced in the study veterans and nearly two-thirds of the veterans on psychoactive medications were able to reduce or discontinue their doses of these medications. Off-label use of FDA blackbox labeled psychoactive medications in veterans with PCS and PTSD has been implicated by NPR/ProPublica in the record suicide rate in veterans. Total deaths from suicides have now exceeded combat deaths. The reduction in depression and suicidality in the Harch study has major implication for this suicide epidemic.
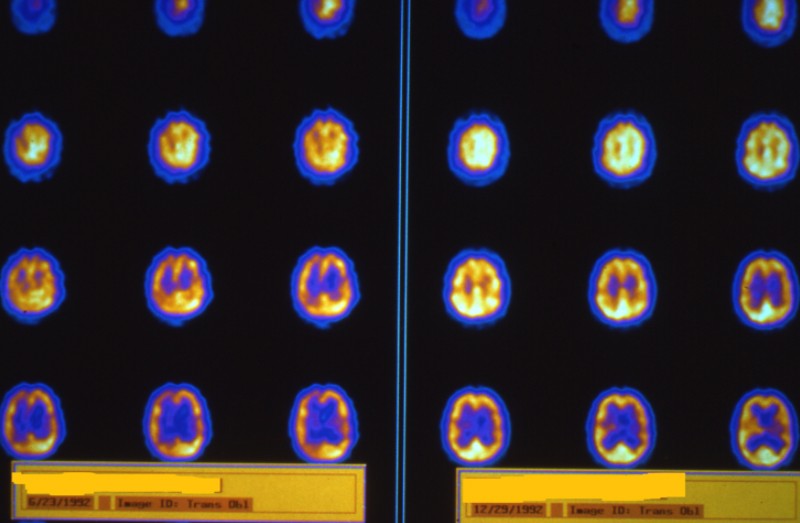
The symptomatic and cognitive findings in the study were fortified and made more compelling by the functional brain imaging performed on the veterans. Dr. Harch and colleagues used high resolution SPECT brain blood flow imaging before and after the first hyperbaric treatment (The Neubauer Effect, pioneered by Richard Neubauer: Lancet, 1990) to test the effect of a single HBOT to predict symptomatic and blood flow improvements after a course of HBOT. The imaging was independently submitted for analysis to a researcher at the University of North Dakota School of Medicine (Dr. Fogarty) and psychiatrist and SPECT expert Dr. Daniel Amen and colleagues (Amen Clinics). Using two different methods of analysis Dr. Harch and colleagues were able to demonstrate significant improvements in brain blood flow after one and 40 HBOTs. The improvement in brain blood flow after the first HBOT involved a shift in the pattern of blood flow that Dr. Harch had used visually for 22 years to predict patients who would improve with repetitive HBOT. Drs. Harch and Fogarty were able to show that this visual pattern shift translated to a statistically significant mathematical change in the blood flow pattern. The researchers were able to also show that the areas of brain with improved blood flow after one treatment overlapped with the areas that showed improvement after 40 HBOTs (the Neubauer Effect).
Most importantly, the imaging analysis was able to prove that the blood flow improvements, and derivatively cognitive improvements, could not be explained by a placebo effect. In SPECT brain imaging placebo studies at most five areas of the brain have been identified to be responsible for placebo effects. After the first HBOT over 85 areas of the veterans’ brains showed highly significant increases in blood flow. After 40 HBOTs additional areas of the brain showed significant improvements in blood flow. These widespread improvements are consistent with the diffuse nature of traumatic brain injury and the known reparative effects of HBOT on chronic wounds. The findings obviated the need for a control group.
The researchers further demonstrated the specific targeting of HBOT to injured areas of brain with highly sophisticated computer techniques. The hippocampus is well known as the region of the brain responsible for short-term memory. It is the first area of the brain injured in a variety of different types of brain injury. Using advanced computerized imaging and statistical parametric mapping Dr. Amen and Derek Taylor, data analyst, were able to anatomically separate the hippocampus from the rest of the brain. In pictures produced in the journal article the researchers were able to show that the hippocampus demonstrated significant improvements in blood flow after the first HBOT with even greater improvements after 40 HBOTs consistent with the significant improvements in memory.
Importantly, the findings in the study duplicated the 22 year concentrated experience of Dr. Harch in the hyperbaric treatment of neurological conditions. This experience was reinforced by the application of the same veterans dose at 1.5 ATA (atmospheres absolute) in an animal model of chronic traumatic brain injury (Brain Research, 2007,www.sciencedirect.com/science/article/pii/S0006899307015612). Dr. Harch and colleagues were able to show an improvement in spatial learning and memory and increased blood vessel density in the injured hippocampus. This animal proof of HBOT in chronic TBI was the first improvement in chronic animal brain injury in science. The findings are nearly identical to the improvements in memory and blood flow in the current veteran TBI study.
The dose of HBOT 1.5 ATA (atmospheres absolute) was first identified by German researchers in acute brain injury, later pioneered by Dr. Richard Neubauer in chronic brain injury, and refined by Drs. Harch, Van Meter, and Gottlieb in sequential 40 treatment blocks for multiple chronic neurological conditions. Beginning in early 2008 Dr. Harch applied this dose to veterans with blast-induced brain injury. The first application to combined PCS and PTSD was published in 2009 by Dr. Harch in BioMed Central’s Cases Journal (http://www.casesjournal.com/content/2/1/6538). The surprising finding was the unexpected improvement in PTSD which was manifest by the 25th HBOT. In the current study the veterans experienced a 30% reduction in PTSD symptoms in one month, a rate of change not seen in PTSD studies with standard of care therapies.
In summary, Dr. Harch and colleagues have shown with just 16 U.S. veterans that HBOT 1.5 is safe, feasible, and remarkably effective in treating the chronic effects of mild blast-induced TBI and PTSD. Headaches, post-concussion symptoms, abnormal neurological exam findings, cognition, quality of life, and brain blood flow were significantly improved after a one month course of HBOT. At six month phone follow-up the great majority of veterans sustained their symptomatic improvements. Many of the veterans sought additional HBOT for further improvement. In comparison to standard of care treatments the Harch study argues strongly for the immediate application of HBOT 1.5 to the hundreds of thousands of veterans with persistent post-concussion syndrome with or without post-traumatic stress disorder.