A traumatic brain injury, also known as a TBI, is an injury that affects how the brain works. They can range in severity. A traumatic brain injury can occur in a variety of ways, so they fall into three categories: mild, moderate, and severe TBIs.
Autism
August 10, 2023Traumatic Brain Injury
Mild TBI
A mild TBI is usually caused by something like a simple fall, sports collision, or hitting the head on a steering wheel. It results in the brain moving around in the skull and a transient alteration in consciousness (seeing stars, dizziness, feeling dazed and confused) for up to 24 hours or loss of consciousness up to 30 minutes. It usually involves some immediate and forward loss of memory for up to one day. An important thing to note is that mild TBIs are still to be taken seriously. A concussion can cause brain damage and serious after-effects. Mild traumatic brain injuries can be even more serious if they continue to happen over and over without medical treatment. This can cause severe symptoms like problems with concentration and memory loss, as well as painful headaches and balance issues. As many as 50% of patients who are diagnosed with mild TBI experience these types of symptoms for days, weeks, or even years after their TBI.

Moderate TBI
A moderate TBI involves a greater degree of force delivered to the head and brain, usually enough to cause bleeding. It is defined by loss of consciousness of 30 minutes to 24 hours and loss of memory for 1-7 days. It can be caused by the same events as mild TBI but involves greater force or the same amount of force as a mild TBI, but delivered to a more vulnerable person such as an elderly person. Generally, moderate TBI patients have more serious and persistent symptoms and greater disability, including problems with thinking, headaches, speech, fatigue, and emotions.
Severe TBI
A severe TBI involves the greatest force, either blunt, such as an unrestrained rollover motor vehicle accident, or penetrating, such as a gunshot, shrapnel, or open skull fracture from an elevated fall. It is defined by loss of consciousness greater than 24 hours, loss of memory greater than 7 days, and other criteria. These patients are the ones who end up in comas on ventilators in ICUs with prolonged recovery times and account for most of the deaths due to TBI. They almost always have symptoms and neurological deficits for the rest of their lives and never return to their previous level of function. The great majority also are unable to work and have significantly reduced quality of life.
Hyperbaric Oxygen Treatment of Traumatic Brain Injury/TBI
As of now, hyperbaric oxygen treatment is the only therapy that directly treats the biological injuries to the brain in TBI patients. HBOT has been proven in multiple studies to reduce the rate of mortality in acute severe TBI patients by as much as 60%. Very few other therapies in the history of mankind have demonstrated this degree of reduction in mortality for any medical illness.
Unfortunately, due to medico-political and economic factors obtaining HBOT for acute severe TBI in any U.S. hospital is nearly impossible. Most patients, if they survive, have to wait to be discharged from the acute care hospital to obtain HBOT. In this subacute phase, however, HBOT is exceedingly helpful.
The best example is the Curt Allen case, a 19-year-old male with a severe TBI who was treated by Dr. Harch four months after his TBI, just a few days after discharge from a rehab hospital where he had experienced no improvement. In chronic severe TBI, HBOT is also extremely helpful. Chronic severe TBI patients were among the first whom Dr. Harch treated in the early 1990s. They experienced significant recovery years after they had stopped making any improvements with traditional therapies.
This treatment is revolutionary in so many ways because it repairs the underlying brain wounds and stimulates the regrowth of blood vessels and brain tissue. HBOT brings new life to patients who have lost theirs. It is hope for the hopeless.
Benefits of HBOT for Traumatic Brain Injury/TBI
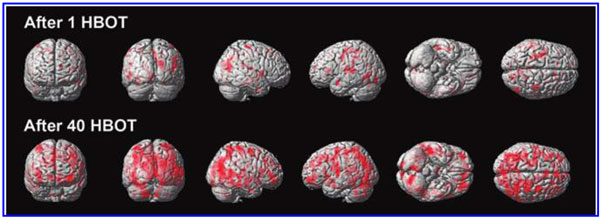
Many patients who receive HBOT as a TBI treatment can experience improvement after only one session. Patients who have suffered from the effects of TBI for many years have shown permanent improvement. Patients with mild TBI have shown marked improvement and, at times, near-complete relief of symptoms in 40 or fewer treatments. This includes relief of headaches, chronic pain, regaining speech skills, and emotional stability as well as helping patients improve their quality of life. The benefits of HBOT for traumatic brain injuries are seemingly inestimable, and more and more patients are experiencing symptom improvement and relief.
Case Study
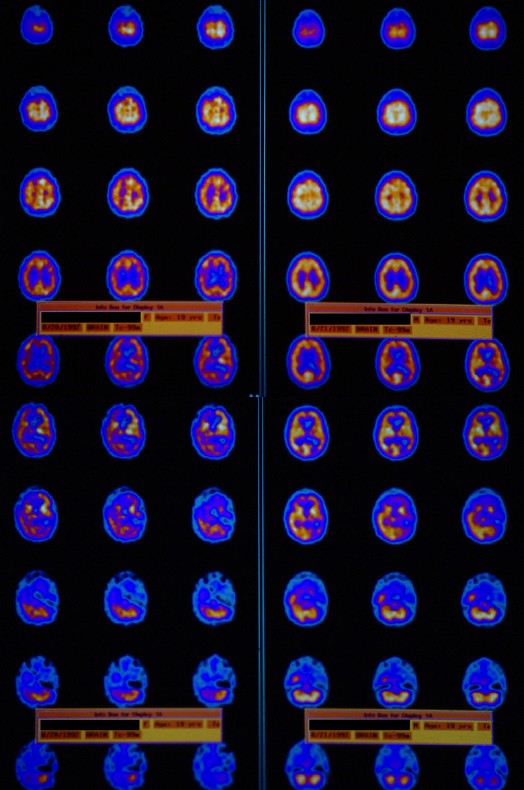
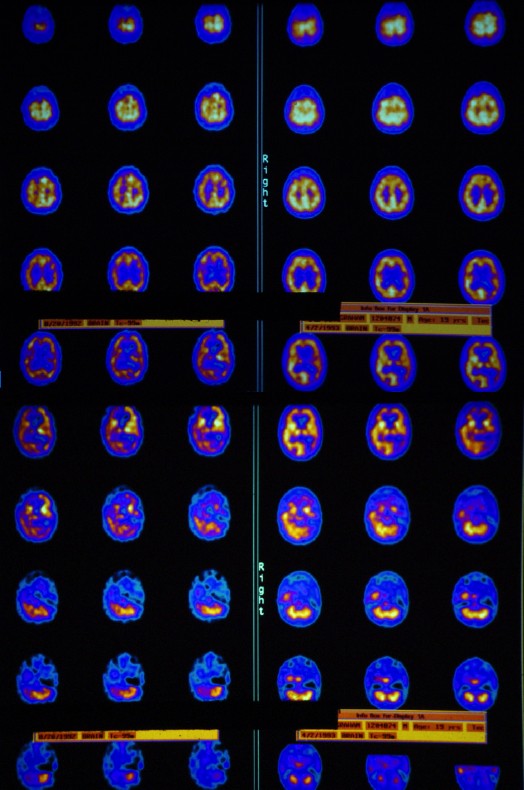
Geoffrey was a 19 year old young man who was involved in a severe motor vehicle accident on an icy winter night in 1989. He was comatose at the scene, spent weeks in the ICU on a ventilator, and then months in a rehabilitation hospital. He was discharged to home and the care of his mother with inappropriate social behavior, cognitive deficits, and repeating sentences in conversation, and he required round-the-clock supervision. His repetitiveness was a particular stressor for his parents, and they were seeking institutional placement for Geoffrey. He was referred for evaluation for HBOT nearly 3 years after his accident.
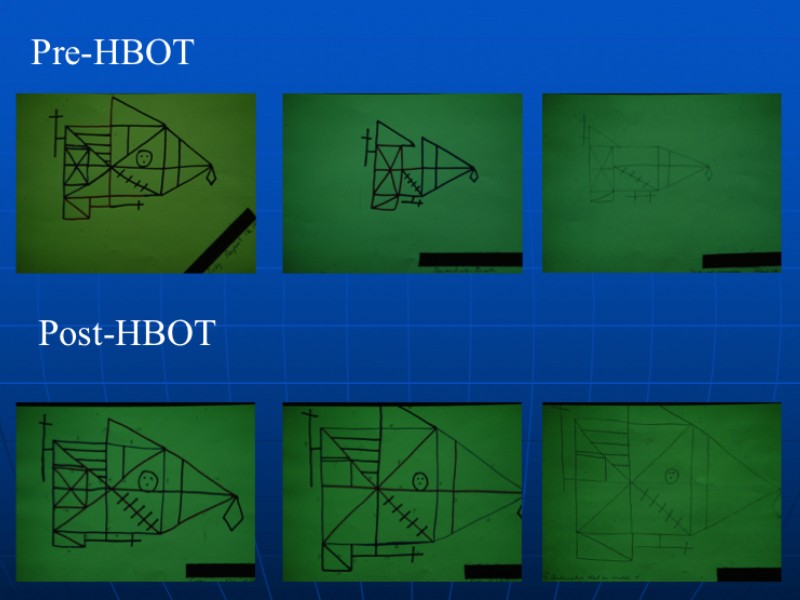
Geoffrey had a SPECT scan, a single HBOT, and a repeat SPECT (see below) which showed a dramatic improvement in brain blood flow. This evaluation was followed by 67 HBOT treatments over the course of the next 8 months, which were delivered in multiple blocks. At the end of treatment, the patient had marked improvement in his behavior, perseveration (repetitive speech), cognitive deficits, and no longer required round-the-clock supervision. Repeat cognitive testing showed improvements in memory and other functions. He was advanced to assisted living and part-time employment. Periodically, Geoffrey returned for additional short courses of HBOT. When asked why he continued to come to New Orleans for HBOT, Geoffrey responded, “I feel so much better in my head and can do new things when I have HBOT.”
Supportive Research and Information
https://www-ncbi-nlm-nih-gov.ezproxy.lsuhsc.edu/pubmed/29132229 (Rockswold review).
https://www-ncbi-nlm-nih-gov.ezproxy.lsuhsc.edu/pubmed/29152209 (Dr. Harch’s study in veterans with blast TBI and PTSD. The discussion section includes a review of all of the HBOT studies in mild TBI persistent post-concussion syndrome).


