Decompression Illness in Divers: A Review of the Literature
August 1, 2011Ronald Mcdonald House Child’s Testimony of HBOT for Brain Trauma
August 24, 2011A Testimony of Hyperbaric Oxygen Therapy By Kathy Summers
HBOT for Angiogenesis
Last summer I broke the neck of my femur clear through (technically a hip fracture) when my horse launched me like a rubber band into the dirt. But that wasn’t the scary part. The fracture was nothing compared to how I felt when the emergency room staff said the words “hip replacement. ”My orthopedic surgeon decided to try setting the bone first, but he gave me slim odds for healing. He said I had almost certainly severed the capillaries that feed the head of the femur, and with no backup blood flow it would begin to die (called avascular necrosis or AVN). When I asked what I could do to prevent this, he said, “Just one thing: hyperbaric oxygen. ”I immediately signed up for 20 daily treatments at Scottsdale Healthcare Osborn in Scottsdale, Arizona.
How HBOT Benefits Maximum Medical Improvement
To benefit from this peculiar therapy all you do is breathe. The key is to breathe 100 percent pure oxygen through a mask or hood for one to two hours a day while sitting in a pressurized chamber. Hyperbaric oxygen therapy (HBOT) works according to a simple law of physics that says oxygen under pressure dissolves into the body’s fluids—including blood plasma, lymph, and cerebral spinal fluid—where it can speed healing.
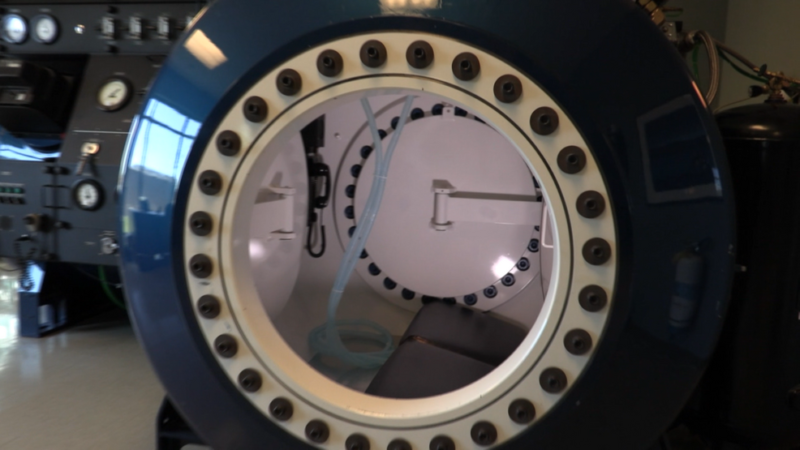
Hyperbaric Chambers
Hyperbaric hospitals and clinics typically operate monoplace chambers that resemble glass coffins, but I shared dives (as they sometimes call the treatments) in a 12-person multiplace chamber that looks like a submarine.
Other than some ear pressure and temperature changes similar to landing in an airplane, the experience is comfortable with no serious side effects.
In cases like mine, HBOT can help the body develop new blood vessels [angiogenesis], remodel bone, and reduce secondary swelling and bruising if it is provided soon enough after the injury or surgery. “When you reduce the inflammatory edema you get rid of the bruising a lot quicker, so you get better circulation to the injured areas,” says Dennis Weiland, MD, Scottsdale Healthcare’s director of hyperbaric medicine. In fact, not only did my deep bruises disappear quickly, I healed completely with no complications and no need for a hip replacement. I was lucky because few orthopedic surgeons refer hip fracture patients for HBOT. Doctors are more likely to prescribe the treatments for wounds that won’t heal.
One of my chamber mates, Brenda Opatz, a 45-year-old single mother of four, received treatments for a nonhealing surgical wound following breast cancer radiation. “My breast surgeon tried everything to get my incision to stay closed,” says Opatz, “but it reopened four different times. After consulting a wound specialist and a plastic surgeon, she prescribed HBOT—and it worked.”
The journal Undersea Hyperbaric Medicine reviewed 74 studies and found HBOT almost always helps in radiation injuries that would otherwise require radical surgical interventions resulting in complications. It also helps heal necrotizing fasciitis (flesh-eating disease) and diabetic gangrene. “We’re not only postponing—we’re preventing amputations,” says Weiland, who is surprised more surgeons don’t prescribe it. “If I were a plastic surgeon doing facelifts, my first post-op order would be to put people in hyperbaric chambers.”
Hyperbaric Oxygen Therapy Treatment is Overlooked
Although HBOT appeared on the medical radar when an anesthesiologist postulated that by increasing the levels of oxygen in operating rooms, patients would heal faster, its applications now include an odd assortment of conditions and diseases it treats, from migraine to crush injuries to near drowning. HBOT’s versatility makes sense only when you look beneath the surface to find the common threads in all the conditions and diseases, explains Paul G. Harch, MD, clinical professor and director of Hyperbaric Medicine Fellowship LSU School of Medicine, New Orleans, and director of the Hyperbaric Medicine Department, Medical Center of Louisiana New Orleans. In other words, whether you’ve injured your brain or your big toe or just had liposuction, if the basic underlying processes include low oxygen (hypoxia), loss of blood flow (ischemia), and/or secondary inflammation, HBOT can potentially help.
HBOT for 14 FDA Approved Conditions
Needless to say, insurance and Medicare won’t cover HBOT for cosmetic surgery. But they also rarely cover it for serious chronic conditions like multiple sclerosis and acute conditions like myocardial infarction (a type of heart attack). Although doctors can and do treat these conditions with HBOT, insurance companies typically only cover the 14 indications approved by the Undersea and Hyperbaric Medical Society (UHMS). That diverse list includes embolism (artery-clogging blood clot), carbon monoxide poisoning, osteomyelitis (a bone disease), and delayed radiation injuries. The UHMS considers all other treatments off-label, although they occasionally make exceptions.
Insurance Coverage for Off-Label HBOT Treatments
Blue Cross Blue Shield of Arizona covered my off-label treatments to prevent AVN, probably because it was more cost-effective to preserve my hip with HBOT than to replace it. The same logic can work for other off-label conditions. But insurance companies steer clear of anything the UHMS considers too controversial, such as traumatic brain injuries. And the UHMS blessing is hard to get. They expect to see a large but unspecified amount of clinical evidence and data proving the treatments work before they will issue an approval for something as common as stroke. “We appreciate that people treat stroke patients with HBOT,” says Weaver, “but unfortunately they have not adequately demonstrated its efficacy in publications.”
That leaves many physicians on the front lines frustrated. “We believe neurology is the future of hyperbaric medicine—it’s the top indication, and it’s not off-label to us,” says the late Richard A. Neubauer, MD, medical director of Ocean Hyperbaric Neurologic Center, Lauderdale-by-the-Sea, Florida. A pioneer in the HBOT industry, Neubauer has contributed the largest body of data on HBOT for neurological disorders in North America. A number of studies show HBOT can reactivate idling neurons in both early and late stages of various brain injuries. Many of the mechanisms are the same as in wound healing.
A small group of dedicated HBOT doctors and researchers have repeatedly applied to the National Institutes of Health (NIH) to fund more studies. In the meantime, they’re also seeking private funding to create a new infrastructure that will push HBOT into the outpatient setting where people can get doctor-attended on- or off-label treatments at affordable rates.
HBOT for Stroke
Until then, people like Valerie Greene, author of Conquering Stroke: How I Fought My Way Back and How You Can Too, will pay out-of-pocket for treatments. After a paralyzing stroke at age 31, Greene began a three-week series of daily HBOT. Her doctors said she’d probably never walk or talk again.
“They were surprised that I even lived because I had a brain stem stroke that cut off the oxygen and blood supply to my brain. Well, I not only walk and talk, I’m a public speaker and a huge advocate for stroke awareness,” says Greene.
Turning up the pressure
While the UHMS defends its conservative position as the way to eventually push HBOT into the mainstream, Harch suggests an alternate solution. To him, thinking in terms of 13 approved indications simply misses the point.
“These are the most disjointed, unrelated group of diagnoses, and as a result, it is difficult for referring physicians to understand,” Harch argues. “If you don’t understand the treatment, you won’t refer patients to it. This lack of understanding is further compounded by the fact that hyperbaric medicine is not taught in medical schools.”
The key, Harch says, is to look at HBOT as a kind of drug—something mainstream medicine is more likely to understand and accept. A series of recent molecular biochemical experiments has shown that, in some situations, HBOT acts as a DNA signaling drug—“possibly the only one we know of that stimulates growth and repair,” he says. Harch expands this perspective in his book, The Oxygen Revolution(Hatherleigh Press, 2007).
If he’s right, the medical community will look at HBOT in a different light. Harch hopes they’ll see how it works as a drug on all the common disease processes underlying the approved conditions. Then they will ask the obvious questions: If it works for these approved conditions and diseases, why not these other conditions with similar disease processes? If it heals radiation wounds, carbon monoxide poisoning, and bone disease, why not traumatic brain injuries or a hip fracture with AVN? Then, Harch predicts, HBOT will truly revolutionize medicine.
Find a Hyperbaric Oxygen Chamber
HBOT is available by prescription at about 600 hospitals and clinics around the US. The fee for each treatment costs approximately $175 to $400 at many outside “free-standing” clinics, compared to $1,000 to $2,500 at most hospitals. Make certain there is a doctor present when receiving HBOT. If your insurance doesn’t cover it, you can submit a claim, when it gets denied submit an “appeal”.
For more information on Hyperbaric Oxygen Therapy call Harch Hyperbarics Inc. at (504) 309-4948
[/vc_column_text][/vc_column]