I. HISTORICAL BACKGROUND
Drs. Paul G. Harch, Paul K. Staab, and Keith Van Meter have developed an innovative program which evaluates patients with traumatic brain injuries (TBI) or brain diseases using SPECT Scan (Single Photon Emission Computerized Tomography) brain imaging and low pressure hyperbaric oxygen therapy (LPHBOT). These brain injury studies were initially conducted under the auspices of the Baromedical Research Institute, a non-profit organization, devoid of shareholders, established by Dr. Van Meter in 1981 to conduct basic, applied, and clinical research in the broad fields of high pressure and critical care medicine. The traumatic brain injury protocol was sanctioned by the Institutional Review Board on Human Research at the Jo Ellen Smith Medical Center, a private, corporate hospital owned by Tenet, located on the West Bank of the Mississippi River in New Orleans, LA from 1993 through May, 1999 when the hospital and IRB closed. This program is now offered as an off-label use of HBOT. The hyperbaric oxygen therapy treatments (dives) are performed at the Family Physicians’ Center, Marrero, LA, a freestanding medical facility owned and operated by Van Meter and Associates – an organization consisting of physicians in New Orleans devoted to the practice of hyperbaric and emergency medicine. The brain scanning is performed, using Dr. Harch’s protocol, on a state-of-technology, high resolution, triple-headed nuclear medicine SPECT scanner at West Jefferson Medical Center, a publicly owned and operated hospital on the West Bank of the Mississippi River in the metropolitan New Orleans area.
The brain injury program is a direct outgrowth of the extensive experience of Dr. Harch treating chronically brain injured patients, the independent 20+ years clinical Hyperbaric experience of Dr. Harch’s practice group (Van Meter and Associates) at the Jo Ellen Smith Medical Center Hyperbaric Medicine Unit, the published reports of Drs. Richard A Neubauer and S.F. Gottlieb, and the 27 year clinical experience with brain injury of Dr. R.A Neubauer in Florida. In the late 1980’s while at the Jo Ellen Smith Hyperbaric Medicine Unit, Dr. Harch observed patients with cerebral decompression sickness and/or air embolism who responded to hyperbaric oxygen therapy long after treatment of inert gas bubbles had passed or with delayed treatment months to years after standard U.S. Navy treatments had achieved partial success. In addition, Dr. Harch observed patients with brain contusion or stroke who, months to years after their neurological injury, concomitantly experienced gratuitous neurological improvement during the course of hyperbaric treatment for one of the standard accepted indications.
II. THEORETICAL CONSIDERATIONS FOR HBOT TREATMENT
Decompression Sickness
Standard diving medicine principles suggest that decompression sickness (DCS) involves bubble formation in the circulatory system thereby interfering with the necessary continuous supply of oxygen and nutrients to the nerve cells in one or more areas of the brain or spinal cord. Minutes to hours after the onset of decompression illness, tissue damage continues to develop because of persistent occlusion of blood vessels by bubbles or secondary damage to the blood vessel caused by passage of the bubbles. The situation is virtually identical to the pathological processes occurring in the brains of people during and after a stroke. Even after the initial trauma to the brain and the initial course of therapy, there may be residual damage to the nerve cells.
The initial HBOT treatments are thought to help remove bubbles from the circulatory system of the brain or spinal cord thereby permitting the circulatory system to carry out the vital functions of continuously supplying oxygen and nutrients to the affected nerve cells and removing their waste products. However, the successful treatment of DCS involves more than just the removal of bubbles; it involves treatment of the downstream tissue damage resulting from interrupted blood flow and oxygen delivery. Repetitive hyperbaric oxygen treatments tend to result in improving the functioning of the tissues and nerves that show residual damage resulting from the trauma. We contend that the progressive improvement in nerve function is due to the hyperbaric oxygen treatment protocols we use. The scanning and treatment protocols we employ not only help us to determine the presence of potentially recoverable nerve cells but also help us to follow the course of therapy and determine when therapy should be stopped.
SPECT IMAGING
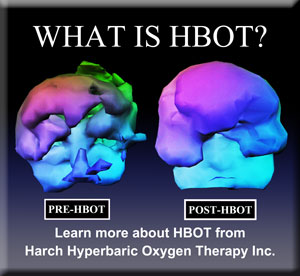
With the advent of clinical SPECT in the 1980’s, physicians, for the first time, were able to see functionally abnormal areas in the brain which were not revealed by standard anatomical brain imaging modalities such as Magnetic Resonance Imaging (MRI) or by X-ray techniques such as CAT scanning (CT). MRI and CT tests only reveal the presence of structural, not functional, changes such as those produced by the presence of dead tissue or swelling. In contrast, brain SPECT images reveal deficiencies in two interrelated functions, blood flow and nerve cell metabolism.
SPECT brain imaging is a simple test that communicates a substantial amount of information about brain function. The procedure involves injecting a minute amount of radioactive material into a vein, usually an arm or hand vein. As the chemical circulates in the body, it is taken up within minutes by brain tissue proportional to blood flow. Once the nerve cells take up the chemical, it remains there for a day. During that time, the radioactivity decays to nothing. One hour after the injection the patient lies motionless on a special scanning table or “couch” around which are arranged sophisticated Geiger counters (cameras) that collect and measure the radioactivity (radioactive counts) over a 15 minute period. The SPECT procedure is non-invasive, painless and considered harmless. It is identical to nuclear medicine procedures performed hundreds of thousands of times all over the United States each weekday by Nuclear Medicine Departments of hospitals and imaging centers, especially on stroke and cardiac patients. A computer reconstructs the radioactive counts to help form functional images of the brain. Those areas of the brain where there is significant abnormal blood flow and nerve cell dysfunction will demonstrate little to no radioactivity
BRAIN INJURY
When traumatic brain injury (TBI) occurs, irrespective of the cause, brain blood flow is either directly or indirectly altered and almost invariably decreased. In the region of the injury, if it is primarily a vascular injury, there is a continuous decrease in blood flow between the high flow at the edge of the wound to the absence of blood flow in the center of the wound. The compromised blood flow implies that there is a simultaneous decrease in blood pressure along the affected blood vessels as well as a decrease in the oxygen delivered to the cells supplied by those affected blood vessels. Significantly decreased blood flow, accompanied by marked decreases in available oxygen, is referred to as ischemia. Research in animals and humans showed that when the available oxygen falls below a certain minimal level, the nerve cells, although alive, become sluggish in their metabolism and can no longer conduct bioelectric impulses. Brain cells which cannot conduct bioelectric impulses behave as if they are dead when tested by conventional techniques. Nerve cells that are metabolically sluggish and electrically non-functioning are called idling neurons. The region of the wound in which idling neurons are located is referred to as the ischemic penumbra. As one proceeds from the ischemic penumbra to the center of the wound, the available oxygen and blood flow drop by an additional 50% and the nerve cells eventually die. The amount of brain tissue that dies depends primarily on the extent of damage to and interference with brain blood flow. With tiny wounds, such as may be seen in certain cases of brain decompression sickness, there is less likelihood that the cells will die. However, with large wounds in the brain, such as occur in major strokes, a fair amount of brain tissue dies. Nothing can be done to revive dead brain cells. However, all brain injuries have varying amounts of ischemic penumbral areas containing idling neurons. Idling neurons may remain quiescent for years.
Recovering idling neurons is the aim of our program.
For the past 27 years Dr. Neubauer in Florida has been using hyperbaric oxygen therapy to treat patients with various neurologic conditions. Although the patients improved, he, unfortunately, was unable to see what was happening to the brain until 1989 when he and Gottlieb used a variation of normal SPECT imaging on a 60 year old woman who had experienced a stroke 14 years previously. They performed two consecutive SPECT brain scans with a single exposure to low pressure hyperbaric oxygen immediately before the second scan. When they compared the after oxygen scan with the before-oxygen scan they noticed that the after-oxygen scan had a greater uptake of the radioactive tracer, i.e. improved blood flow, and, thereby, a decrease in the brain injury. They interpreted these facts to mean that the oxygen improved brain function by increasing the metabolism of the idling neurons. After 60 hyperbaric oxygen treatments, administered over the next 18 months, they were able to recover a fair amount of neurological function in this patient even though the therapy was started 14 years after her stroke. Drs. Neubauer and Gottlieb published this report and two additional cases of near drowning and natural gas poisoning. i ii iii
Subsequently, Drs. Harch and Van Meter, at the Jo Ellen Smith Hyperbaric Medicine Unit, performed the same sequence of SPECT scan! HBOT/SPECT scans on commercial divers with brain decompression sickness and obtained results similar to those of Neubauer and Gottlieb. iv v vi
This growing body of prospective experience provided the explanation for the phenomena described earlier at the Jo Ellen Smith Medical Center Hyperbaric Unit, where patients with neurological problems who were treated for accepted hyperbaric indications experienced gratuitous neurological improvement as their hyperbaric treatment progressed. Unfortunately, at that time, this specialized brain imaging technique was not available to document the neurological changes.
III. BRAIN INJURY PROGRAM – HBOT FOR TBI
Based on the increasing body of knowledge independently obtained by the medical investigators in Florida and Louisiana, Drs. Harch, Van Meter, Gottlieb, and Staab, through the Baromedical Research Institute, started a study to examine the effects of hyperbaric oxygen and SPECT scanning on diagnosing and treating any neurological condition that is associated with decreases in brain blood flow and metabolism on SPECT brain scan. This study effectively indexed and correlated measurement of neurological function and the effects of HBOT to improvement in brain blood flow on SPECT scan. Under ideal conditions, the investigators would have performed a randomized, prospective study with all appropriate controls. However, they did not have the vast financial resources required to support such an extensive and detailed investigation. Because of the large number of brain injuries in the United States and their firm conviction that HBOT is a valuable therapy for treating neurological injuries and diseases, Drs. Harch, Van Meter, Gottlieb, and Staab developed a way of working around the financial obstacle by collecting preliminary data for each separate neurological disorder using a small patient series. Although the program was termed experimental, it was based on sound scientific principles and practices and when delivered in a private physician’s office or hospital also known as the Off-label use of the accepted drug HBOT. To increase the significance of their data, they excluded patients whose brain injury was less than a year old. By so doing, they were trying to avoid arguments claiming that the favorable results that they obtained were due to spontaneous improvement. Now with duplication of their findings by other institutions vii they know these results were not due to spontaneous improvement. In addition, with the termination of that previous study, treatment is no longer restricted to those with chronic injuries and Dr. Harch is now able to treat patients immediately post-injury when maximum benefits can be achieved.
HOW OXYGEN WORKS
The exact mechanism whereby oxygen exerts its beneficial effects on the brain is not known. The physicians think that oxygen is working in the brain in a fashion similar to the way it works in the treatment of other wounds. In the body oxygen is known to stimulate:
the metabolism of nerve cells that have been deprived of oxygen;
the removal of toxic metabolic products;
the efficiency of cells that clean out damaged and dead tissue;
the number of cells that produce new connective tissue in the cleaned out areas;
the amount of new connective tissue to fill in the empty spaces;
the formation of new blood vessels that will provide a continuous source of oxygen, nutrients and the removal of waste products for all the new cells that have been formed.
RISKS OF HYPERBARIC OXYGEN THERAPY
The risks primarily are those associated with hyperbaric oxygen therapy. These risks are generally minimal. The only persons to be excluded from treatment would be those who are actively wheezing or who have asthma. Patients with seizure disorders will be evaluated on an individual basis. One of the most common risks involves changes in pressure in the middle ear: these changes are somewhat more exaggerated than the effect one experiences during take-off or landing of a commercial airplane. In patients who cannot “clear their ears,” such as children or those severely brain injured, mild pain and fluid accumulation may occur in the middle ear space. This can cause some temporary decrease in hearing which will clear in one to two weeks. Those patients who cannot clear, who develop fluid accumulation, and decide to enter the treatment program would require pressure equalization tubes–the tiny plastic hollow ear tubes that are often placed in children who have chronic ear infections.
Please be aware that the vast majority of patients that are treated with hyperbaric oxygen therapy throughout the world are people with diabetes who, at the same time, may have a variety of other ailments such as heart, kidney, brain, vascular, and metabolic disease. Complications associated with hyperbaric oxygen therapy are exceedingly rare. In approximately one quarter of the brain injured patients, however, there is another effect that has been noticed in New Orleans, namely, a change in emotional state usually occurring during the first two to four weeks of treatment. Patients, who, after their injury, became very quiet, can have emotional lability, bouts of crying, irritability, temper tantrums, decreased emotional control, and swings of mood, indicating a change in brain function. In all likelihood this change represents an improvement in nerve cell function brought about by an oxygen-induced increase in blood flow with its improvement of local oxygen delivery and removal of metabolic waste products. It has been observed that this emotional change is temporary and improves with further treatment in the next few weeks. Based on our experience, we strongly recommend against discontinuing treatment during this period or adding medication to control behavior.
In contrast to the above mentioned quiet patients, it has been observed that those patients who, after injury, became more uninhibited and aggressive tended to regain control. This change tended to be a more permanent effect which persisted beyond discontinuation of HBOT.
IV. PROCEDURES FOR ENTRY INTO THE HBOT FOR TBI PROGRAM
If, after carefully reading this material, you desire an evaluation by scan-dive-scan and then possibly treatment, the process is as follows:
- Contact Dr. Harch’s office (504-309-4948) and advise the office staff of your intentions. The staff will begin scheduling appointments and tests based on your intentions. Phone interviews with Dr. Harch can be scheduled at this time. In addition, decisions will be made as to what pre-dive laboratory tests are necessary, if any.
- Formal referral from your physician. This is OPTIONAL. Dr. Harch does not require referral from anyone or by anyone; however some patients’ insurance plans require this for insurance or other third party reimbursement of consults, treatments, imaging, etc. Please check with your reimbursement source. If formal referral is required Dr. Harch will be happy to work with you and is willing to speak with your physician(s) regarding his program before asking for any formal consult. You can notify your physician that the referral is solely for an opinion by Dr. Harch. Dr. Harch will order any tests, imaging, and treatment described above.
- Scan, dive, scan sequence is scheduled with a minimum 24 hours between the injection for the first scan and injection for the second scan. The usual sequence is evaluation by Dr. Harch on the first day, SPECT brain imaging that afternoon, first HBOT the following morning, repeat SPECT at a specific time after the HBOT. Dr. Harch must evaluate all patients before the hyperbaric oxygen dive and usually before the first SPECT scan, especially if the patient needs sedation. It is important to minimize problems since the expenses involved with out-of-state patients are significant.
- Dr. Harch’s office and the Family Physicians Center HBO technician will send confirmation of appointment times and maps with directions.
- Notify Dr. Harch’s office staff and the Family Physicians Center HBO technician of your planned location of stay in New Orleans, phone number at that location, as well as cell, home, and work phone numbers before arrival so that we may contact you regarding any changes in scheduling.
- If appropriate, obtain any pertinent laboratory and imaging results and send them along with copies of other pertinent medical records to Dr. Harch for him to review before you arrive in New Orleans for consultation.
- If available and possible, please bring copies of the patient’s most recent brain MRI or CT scan as well as the reports to Dr. Harch.
- It is recommended that all patients undergo a short video interview and exam with the patient’s and/or their parents’ permission. This has been an integral part of Dr. Harch’s evaluation procedure since the outset of this program, but it is OPTIONAL. Video can capture subtle and not so subtle abnormalities that are often difficult to record with routine history and physical exam. The power of such a video record is evident in two videos placed on YouTube by the father of one of Dr. Harch’s patients (Go to YouTube and search Dr. Harch, Curt Allen, or Chad Rovira). These videos were featured in an AMA News article on the use of video in medical evaluations in 2007. The video will serve as a baseline evaluation from which post treatment evaluations will be compared on video. This is helpful documentary evidence of treatment effect and may be useful to insurance companies. It is also a formal part of the medical record and is as confidential and private as any other part of the medical record. For patients involved in litigation this video can be subpoenaed as part of the medical record file. If you do not desire a video let Dr. Harch know at the time of the evaluation. Your decision will have no bearing on consultation or treatment.
- For those who request and schedule a scan, dive, scan sequence Dr. Harch will review the scans with all interested parties after the final processed scans are returned to Dr. Harch. If there is evidence of improvement, hyperbaric oxygen therapy will be very strongly recommended. If blinded reading by Dr. Harch shows deterioration in the after-dive scan Dr. Harch will discuss the implications of this finding based on his experience with patients who subsequently underwent a course of HBOT. For those patients who do not undergo scanning, treatment can be provided identical to those who do undergo scanning. Please bear in mind that Dr. Harch is one of the only facilities using SPECT brain imaging in conjunction with hyperbaric oxygen therapy. The extensive experience with this imaging modality over the past 20 years has obviated the necessity of using the scan, dive, scan sequence in most patients and has allowed predictive statements in a variety of neurological diagnoses without imaging. Dr. Harch is happy to treat on this empirical basis without imaging. It’s the patient’s choice.
- In those patients who have difficulty clearing their ears on the initial dive, a variety of measures will be attempted to facilitate subsequent ear clearing. If these measures fail PE tube placement will be necessary before further hyperbaric treatment.
- This treatment program may result in charges that may not be recoverable from third party carriers. Patients are responsible for these charges. Evaluations by Dr. Harch during treatment and formal re-evaluations after treatment blocks will be billed to the patient’s reimbursement source by Computed Progress. Payment from this source will be accepted as payment in full unless rules of reimbursement require otherwise, e.g. Medicare.
- It is requested and recommended that all patients receiving treatments undergo a minimum of 40 treatments. In Dr. Harch’s experience less than this is inadequate and seriously compromises permanent effects of HBOT. Treatments are given five days per week. These can be done on a twice a day basis if tolerated by the patient. You will need to plan on staying in New Orleans for the duration of 40 HBOT treatments.
- If no change occurs by 40 HBOT treatments we may not recommend and you may not desire further treatment. This will be discussed at length with you by Dr. Harch.
- If positive changes have been experienced Dr. Harch will also discuss further treatment based on his experience and the medical literature.
- Please bring a short summary medical history if possible. For those patients with extensive medical histories, try to be brief. If possible, put your medical history in chronological order, even bullet form, beginning with the first date the symptoms appeared and then date subsequent entries as new symptoms develop and medical tests are performed. Note the results of the tests and results of consultation with various doctors up to the time of presentation in New Orleans. This is helpful and will facilitate exchange of information during your visit with Dr. Harch, but is not mandatory. Greater detail can be added at the time of the history and physical.Please bring the results of any neuropsychological testing. If this testing has not been performed Dr. Harch will discuss whether this is necessary in your case. Should neuropsychological testing be necessary and/or requested by the patient Dr. Harch can order this in New Orleans, but this needs to be scheduled 3-4 weeks in advance of your arrival. In cases involving litigation this is often a critical piece of documentation that is indispensable before and after treatment. It may also help with third party reimbursement of treatment.
V. RESULTS TO DATE
As of January 2009, the great majority of patients diagnosed and treated under this program have experienced clinical neurological and cognitive improvement that coincides with improvement in brain metabolism and brain blood flow on final SPECT scans. In Dr. Harch’s experience different neurological diagnoses have different sensitivity to hyperbaric oxygen therapy. Some diagnoses have near uniform positive response to treatment while others can have minimal. Dr. Harch will be very candid about the different diagnoses and their responsiveness so you can make a decision on probability of improvement with HBOT. The basic effect of low pressure HBOT on chronic brain injury has now been replicated in an animal model of chronic traumatic brain injury that Dr. Harch published in Brain Research, 2007.
For additional information please obtain Dr. Harch’s book, The Oxygen Revolution: Hyperbaric Oxygen Therapy: The Groundbreaking New Treatment for Stroke, Alzheimer’s, Parkinson’s, Arthritis, Autism, Learning Disabilities and More.
Dr. Harch’s three congressional testimonies:
Autism and Persistent Development Delay are posted on www.hyperbaricmedicalassociation.org under “congressional testimonies” where a variety of Dr. Harch’s cases are presented with SPECT brain imaging.
Thank you.
Paul G. Harch, M.D.
Copyright Updated January, 2009
References
- Neubauer RA, Gottlieb SF, Kagan RL (1990): Enhancing “idling” neurons. Lancet 335:542.
- Neubauer RA, Gottlieb SF, Miale A, Jr. 1992): Identification of hypometabolic areas in the brain using brain imaging and hyperbaric oxygen. Clin Nucl Med 1992;17(6):477-481.
- Neubauer RA (1990). Severe natural gas poisoning successfully treated with hyperbaric oxygen-2 years later. Presented in Prague, Yugoslavia, Proceedings of the 5th International Congress on Neurotoxicology and Occupational Neurology, Sept 24-27, 1990, page 10.
- Harch PG, Van Meter KW, Gottlieb SF, Staab P. HMPAO SPECT brain imaging of acute CO poisoning and delayed neuropsychological sequelae (DNSS). Undersea & Hyperbaric Medicine, 1994;21(Suppl):15.
- Harch PG, Van Meter KW, Gottlieb SF, Staab P. The effect of HBOT tailing treatment on neurological residual and SPECT brain images in type II (cerebral) DCI/CAGE. Undersea & Hyperbaric Medicine, 1994; 21(Suppl):22-23.
- Harch PG, Gottlieb SF, Van Meter KW, Staab P. HMPAO SPECT brain imaging and low pressure HBOT in the diagnosis and treatment of chronic traumatic, ischemic, hypoxic and anoxic encephalopathies. Undersea & Hyperbaric Medicine, 1994;21(Suppl):30
- Barrett KF, Masel BE, Harch PG, Ingram F, Corson KP, Mader JT Cerebral Blood Flow Changes and Cognitive Improvement in Chronic Stable Traumatic Brain Injuries Treated with Hyperbaric Oxygen Therapy. Neurology, Aprill998; (Suppl) Al78-Al79.


