Low pressure [< 2.0 ATA (atmospheres absolute)] hyperbaric oxygen therapy (HBOT) has been increasingly applied to chronic pediatric neurological conditions amidst much controversy and criticism. The negative reaction by the medical community is due, in large part, to the misconception and confusion of the scientific basis underlying the improvements in patients and the inconsistency of the definition and dosage of HBOT. These controversies are examined by developing the science of HBOT based on the drug definition of hyperbaric oxygen therapy and concept of dose.
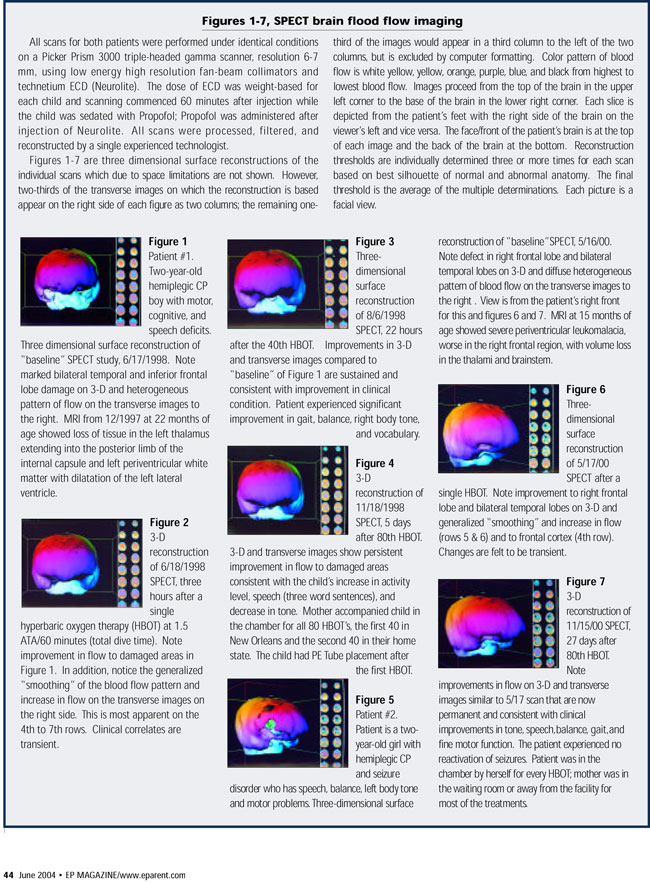
This article will review the current literature and history of application of low pressure (low dosage) LPHBOT to pediatric neurology. The most rigorous study on this subject will be analyzed and its interpretation debated in terms of past and present scientific data and theoretical considerations. The major flaw in the study’s conclusion is illustrated by pre and post HBOT SPECT brain imaging on two of the author’s cerebral palsy patients and the author’s 12-year-experiehce of HBOT treatment of Cerebral Palsy children. There is substantial scientific explanation and data to argue for reimbursement of HBOT in Cerebral Palsy.
Introduction
Since 1998, the international pediatric neurological community has seen an explosion in the off-label use of LPHBOT for chronic pediatric neurological conditions. The reaction of the neurological community has been a mixture of resentment, bewilderment, criticism, misperception, and confusion, largely as a result of a lack of understanding of hyperbaric oxygen therapy and the scientific basis of LPHBOT in chronic neurological conditions.
In 2001 Guo enumerated a variety of reasons for the lack of awareness of hyperbaric oxygen therapy. They included: a lack of evidence, incompatibility with standards of care, the longtime course to see results (weeks to months), inadequate communication of results, and inability to access adopters and payers. In an effort to better understand this patient-driven movement and service these five problems this article will review the science of LPHBOT and the history of development of LPHBOT in chronic neurological conditions. This review will provide a framework for better appreciating and understanding the claims of effectiveness and potential for LPHBOT in chronic pediatric neurological conditions. In addition, it will strongly argue for reimbursement of hyperbaric oxygen therapy in Cerebral Palsy.
Definition
Most of the misunderstanding of LPHBOT in chronic pediatric neurological conditions has been due to the inadequacy of the popular definitions of hyperbaric oxygen therapy. As an example, through 2003 the HBOT Committee of the Undersea and Hyperbaric Medical Society defined HBOT as: “Hyperbaric oxygen therapy (HBOT) treatment, in which a patient breathes 100 percent oxygen intermittently while inside a treatment chamber at a pressure higher than sea level pressure (i.e., > 1 atmosphere absolute; atm abs), can be viewed as the new application of an old, established technology to help resolve certain recalcitrant, expensive, or otherwise hopeless medical problems.” Careful scrutiny reveals that this is a non-definition. Further, it misleads people into believing that HBOT is exclusively a “hail Mary” attempt at ameliorating recalcitrant medical conditions. Because of this non-definition the Accepted Indications List [Table 1], compiled by the same committee, appears to physicians and non-physicians alike as a random compilation of medical diagnoses. The non-definition and list robs the therapy of an understanding of its physiology. The net result is gross confusion when individuals are referred to this list and the HBOT Committee Report as the foundation source material on HBOT. When cerebral palsy is unofficially added to the list the confusion is compounded. As a result, HBOT has been referred to in the past as “a therapy in search of diseases.”
A more precise definition of HBOT is the drug definition, first proposed by Gottlieb and later refined/focused by Harch and Neubauer as the use of greater than atmospheric pressure oxygen to treat basic disease processes and their diseases. In essence, HBOT acts as a drug on the underlying basic pathophysiologic processes and states of a cell, tissue, organ, or organism and through these effects treats the disease itself. Referring back to the Committee Report’s Accepted Indications List, there is a plethora of animal and basic science studies documenting unequivocal actions of HBOT on acute and chronic disease pathophysiology, and hence the diseases on the list.
Many of these actions result from the direct effects of oxygen on blood vessels, cell surface proteins, enzymes, and DNA, or through its properties and behavior according to the Universal Gas Laws. In many diseases one or more timely high-pressure HBOT’s can have curative or dramatic ameliorating effects. In chronic conditions HBOT drug effects are tissue, blood vessel, bone, and skin growth/repair.
The prototypic HBOT model in chronic wounding is the shallow blood flow/oxygen gradient wound of external beam radiation for cancer described by Marx. Daily HBOT in these chronic wounds generates new tissue and blood vessel growth that proceeds from the edge of the wound to the center. Tissue growth requires new protein which results from stimulation of the cells’ DNA. The exact molecular mechanisms of action have remained elusive until recently.

In the past six years molecular biochemical studies have shown that daily exposures to HBOT signal the DNA of cells in a chronic wound to repair and grow new tissue. Using the drug definition of HBOT and the knowledge of acute and chronic HBOT drug effects the Accepted Indications list now becomes a set of diagnoses connected by HBOT effects on common underlying pathophysiologic processes, i.e. the definition given above.
The drug definition of HBOT entails the concept of dose. HBOT dose is a function of depth of pressurization, amount of time at pressure, presence or absence of air breaks, frequency of treatments, number of treatments, and the nature of the underlying pathology which is defined by the time of intervention of HBOT in the disease process. In hyperacute CNS (central nervous system) and non-CNS conditions and in chronic non CNS wounding (e.g. diabetic foot wounds), high pressure (greater than or equal to 2.0 ATA), HBOT is effective. (Sea level pressure is 1· ATA; each additional atmosphere of pressure is equivalent to 33 feet of seawater pressure if one was breathing air underwater). In CNS injury, however, as one proceeds beyond three to six hours the highest pressures may not be effective and by 48 hours can be toxic, i.e., an overdose. At this time injured brain appears to be responsive to pressures less than or equal to 2.0 ATA, and after one month or more almost exclusively less than 2.0 ATA. While the above is a synthesis of hyperbaric literature over the past forty years, the discovery of this tapering of dose was made in the late 1980’s in New Orleans while treating divers with brain decompression illness (DCI). Out of this experience grew the application to chronic pediatric brain injury. A brief recitation of this history will be helpful.
History
The standard of care for treatment of acute DCI has been repetitive high (2.0·2.8 ATA) pressure oxygen treatments. In the late 1980’s we found that divers gained further neurological improvement if the treatment pressure was lowered to 1.5 ATA. In addition, we found that divers delayed weeks or months to first treatment or who failed standard Navy treatment months to years before could be successfully treated at the same 1.5 ATA, similar to Neubauer’s treatment of chronic stroke and multiple sclerosis patients. In these cases it was obvious that subacute and chronically injured brain tissue was the primary pathology, not residual free inert gas. We then extended this 1.5 ATA HBOT to boxers and patients with chronic traumatic brain injury, stroke, toxic brain injury, autism etc., and placed the work under a hospital based human experimentation committee (Institutional Review Board-IRB) approved protocol. Evaluation of patients for LPHBOT was based on the sequence of high resolution SPECT brain blood flow scan, single LPHBOT, and repeat SPECT. Before opening the IRB one of the early referred patients in 1992 was the first cerebral palsy child treated with HBOT in North America The patient was a four-and-a-half-year-old boy with hypotonia who couldn’t walk. At the end of three months the child experienced improvement in fine motor function, alertness, and walked with fingertip support for balance; subtle improvements were noticed on SPECT. Through the closure of the IRB in May 1999 approximately 50-75 children and 150 adults were evaluated and treated for chronic brain injury. Some of the pediatric cases were reported at the First, Second, and Third International Symposia on Hyperbaric Oxygenation and the Brain Injured Child in July 1999, 2001, and 2003.
Unbeknownst to me, however, the use of LPHBOT predated the New Orleans experience by a decade; Dr. Machado in Brazil treated 230 children from 1983 to 1989 using an identical pressure with lesser number of treatments, yet the same qualitative results. He presented his findings at a conference held by Dr. Richard Neubauer in Fort Lauderdale, Florida in 1989. Dr. Machado’s protocol was 100 percent oxygen at 1.5 ATA/60 minutes total dive time (TDT) for 20 treatments in a monoplace chamber. Subsequent experience will be referenced to this dose.
Following the first child above and eight additional children with static encephalopathy of various causes treated in New Orleans. a child from Wisconsin was treated with LPHBOT in South Florida in late 1995. The child was a severe quadriplegic who experienced improvement in tone and alertness. Her case, and two of my own, were presented at The Third Panamerican Congress on Hyperbaric Medicine in Rio De Janeiro, . April, 1996. Simultaneously, the first Cerebral Palsy children were treated in Sussex England. By 1997 a number of mothers from Montreal took their children to Sussex, for the same treatment and pediatric physiatrist Dr. Pierre Marois of L’Enfant Hospital of Montreal noted a significant decrease in spasticity of two twin four-year-old boys with quad Cerebral Palsy. This prompted fundraising by a group of mothers to launch the McGill Pilot Trial where patients served as their own controls. The positive results of this study generated the government funded multicenter McGill trial recently published. The confusing results of this trial become explicable when discussed in terms of dose of HBOT and DNA signaling.
The pressure and dose of HBOT in Brazil was 1.5 ATA of 100 percent oxygen for 60 minutes TDT. In New Orleans it was originally 1.5/90 minutes, but then reduced to 1.5/60 minutes TDT when patients developed side effects from the extra 30 minutes in chamber. Due to non-physician attendance, free-standing HBOT centers in the U.K. use 95 percent oxygen; the dose in Sussex was 20 HBOT’s of 95 percent oxygen at 1.75 ATA (1.66 ATA oxygen)/60 minutes at depth. When the McGill Pilot Trial commenced the dose was increased to 20 treatments of 100 percent oxygen at 1.75 ATA/60 minutes at depth. While the Gross Motor Functional Measures (GMFM) improved in many of these children, Dr. Marois noted that the children experienced regression of some of their symptoms upon cessation of HBOT. In my nine years’ experience prior to this result, it was found that permanence to LPHBOT-induced neurological improvements was achieved beyond 35 treatments. (Congruently, and incidentally, the average number of HBOT treatments delivered to patients in the U.S. with non-CNS wounds is approximately 40 and the minimum dose to patients with non-CNS radiation injury wounds is 40.)
This was communicated to Dr. Marois and the multicenter trial became 40 LPHBOT treatments at 1.75 ATA of 100 percent oxygen/60 minutes at depth. While this was the correct number of treatments the 1.75 ATA 100 percent oxygen 60 minutes AT DEPTH was a higher dose never before applied to Cerebral Palsy children. Simultaneously, despite warnings to the contrary, the control group was chosen to receive 1.3 ATA air or essentially .27-.28 ATA oxygen at pressure, a 30 percent increase of oxygen over sea-level air. Thus, this was not a true control group, nor was it a control group ever before used in HBOT clinical studies. Unfortunately, this is the root of the study’s confusion and misinterpretation.
Discussion
The medical community has misinterpreted the results of the rigorous McGill Multicenter Trial for a variety of reasons. First, the improvement of the hyperbaric oxygen therapy group is entirely consistent with the observations of the Russians, Machado, myself, Neubauer, the McGill Pilot Trial, and the subsequent independent reports from practitioners and investigators in China, Bulgaria. Yugoslavia, South Africa, Italy, Germany, the U.K., Canada, the United States, Mexico, and South America All of these reports are consistent with HBOT oxygen signaling effects on injured brain tissue in shallow blood flow/oxygen gradient wounds. These gains were far greater and in a shorter period of time than has been seen with spontaneous changes in GMFM. The GMFM scores showed the effect of possible oxygen toxicity or metabolic fatigue suppression of scores at 1.75 ATA as evidenced by improvement in 5 of the 6 scores in the HBOT group from the immediate post-testing period to the three month post hyperbaric oxygen therapy testing; only 3 of the 6 improved in the control group. The improvement in the control group is the confounder that has misled the scientific community. The article attributed the improvement in the controls to a parent participation effect. Using the argument of oxygen signaling, a more plausible conclusion is that the chronically injured pediatric brain is exquisitely sensitive to intermittent oxygen signaling at low levels of hyperbaric pressure and oxygen.
Four separate lines of evidence support the “sensitivity” argument. First, Chinese researchers just reported in an acute model of Cerebral Palsy that hyperbaric air causes an increase in a brain growth hormone while hyperbaric oxygen therapy causes an increase in the hormone plus a DNA messenger substance that results in new protein production, i.e. oxygen DNA signaling. Second, the Bulgarians and Russians have both reported beneficial effects of low pressure hyperbaric air and oxygen mixtures on children with Cerebral Palsy. Third, Heuser reported beneficial effects of low-pressure hyperbaric air on children with chronic toxic brain injury. Lastly, the brain is composed of gaseous neurotransmitters, e.g., carbon monoxide, nitric oxide, etc. and mitochondrial pressure sensitive molecules whose behavior is poorly documented under hyperbaric conditions, but in fact may contribute in some way to neurological changes in a patient.
The opposite arguments of placebo or parent-accompanying effects are specious. 1b be a placebo a substance must be inert and to have a placebo effect the subject must of capable of understanding that the treatment can have either a positive or negative effect on him/her. By definition neither oxygen nor hyperbaric oxygen can ever be placebos due to their physical properties alone. Secondly, in younger children and those damaged enough to not appreciate suggestion placebo requirements can similarly not be fulfilled. If anything a negative placebo effect would be present due to the “white coat effect” and the fright of yet another medical intervention in these children. In addition, many of these children have been subjected to every conceivable medical therapy over the course of their short lifetimes and the parents and researchers have never witnessed this degree of improvement in two short months.
This last rebuttal can also be applied to the parent participation effect argument. If quality time with the kids in an atmosphere of good cheer can cause such a rapid improvement in gross motor function why hasn’t it done so in all of the previous therapies? In my research and practice with 170 children we have eliminated this argument by design default, using single-person chambers and having over 85-90 percent of our children dive alone while watching a Barney or similar video; the relatives or parents are out of view in the lobby or absent from the facility. One could argue the placebo effects of a Barney video, but due to their ubiquity all parents of Cerebral Palsy children should have seen big gains with such videos at home. In fact, they haven’t. A recent review on placebo effects demonstrated that no significant objective outcomes, such as were seen in this study, could be attributed to placebo. Another study on HBOT “placebo” effects in adults demonstrated that any placebo effects are those of anxiety reduction and mood elevation, not durable neurological effects.
Since the publishing of the Collett article additional work by Waalkes, Golden (Neubauer), this author, and Sethi render the sensitivity and non-placebo arguments somewhat moot. All four authors have shown significant improvements in function and/or SPECT brain imaging treating Cerebral Palsy children with similar low pressure hyperbaric oxygen therapy protocols. The last study by Sethi was a randomized prospective controlled trial without confusing dose issues that was awarded first place at a scientific meeting in India. Collectively, the evidence for a beneficial effect of hyperbaric oxygen therapy in Cerebral Palsy now exceeds nearly all of the 13 Accepted Indications.
Theoretical Considerations
Setting aside the above clinical experience, is it plausible that LPHBOT could benefit the cerebral palsy brain? The answer is yes, and turns on the existence of chronic shallow blood flow/oxygen gradient wounds in Cerebral Palsy similar to the extremity wounds hyperbaric oxygen therapy has traditionally treat-ed. Innumerable SPECT blood flow studies have shown that such wounds exist in adult human brains. There is also evidence in pediatric brain injury. It is known that Cerebral Palsy is largely a vascular or low blood flow/oxygen insult, depending on the age of the child and/or degree of prematurity at time of injury, and has been registered on SPECT and PET. It is only reasonable given the mechanism of HBOT described above in radiation wounds that HBOT in the proper dosage could rehabilitate a brain wound just like a neck or leg wound. Twoexamples from our previous IRB experience (vide supra) show SPECT registration of these shallow blood flow/oxygen wounds in Cerebral Palsy, the rehabilitation of these wounds with LPHBOT and the lack of a parent participation effect on these images and the patients’ concomitant clinical improvement (Figures 1-7). Both cases demonstrate innumerable shallow perfusion gradient wounds that improve after both single and repetitive LPHBOT. The effect is the same regardless of parent accompaniment on every LPHBOT, patient #1, or the child diving alone, patient #2. This is also the same effect we have continued to see to this day in the great majority of nearly 175 children with chronic neurological disorders of which 80 percent have been imaged with SPECT.
Probably the most compelling piece of evidence arguing for a scientific basis for the beneficial effect of hyperbaric oxygen therapy in Cerebral Palsy and chronic brain injury is additional animal work. After criticism of my chronic case series of divers, trauma, toxic, and other brain injured patients mentioned above, I sought duplication of this work in an animal model in 1995. In a controlled pilot trial of 12 rats with chronic traumatic brain injury we demonstrated statistically significant improvement in cognition and simultaneous increases in blood vessel density. In June 2001 these findings were replicated in a much larger number of rats with greater statistical significance, achieving the first demonstration of non-invasive improvement of chronic brain injury in an animal model. These experiments employed the original human protocol used in the first divers and Cerebral Palsy patient above. While the model is different, trauma vs. low blood flow/oxygen, the results were consistent with all of our previous findings and that of others in multiple human conditions. In addition, it strongly argues for a scientific basis for the human experience.
Controversy
Finally, a few words about entrepreneurs and exploitation; it has been stated that HBOT is “big business.” Such statements belie ignorance of the economics of HBOT. On April 1, 2003 the Center for Medicare/Medicaid Services (CMS) doubled the reimbursement for hyperbaric oxygen therapy that, when added to the patient’s copayment and the physician fee, brings the total to about $420/60 minute treatment. Since the treatment for accepted indications is usually 90-120 minutes the total reimbursement exceeds $600.00. The average freestanding facility charge for off-label HBOT in the U.S. and Canada in non-physician attended facilities is about $75-125/treatment and this is largely non-reimbursed by third party payors. In physician attended facilities it is $150-200/treatment. There are currently less than five full-time physician attended facilities in the United States that are exclusively treating off-label diagnoses. Meanwhile, there are approximately 130 or so non-physician attended facilities in the U.S. and Canada doing the same. In contrast hospital facilities charge $1,000-$3,300/treatment for “accepted indications.” Where’s the bonanza in freestanding off-label use of HBOT? There is none.
The criticism of exploitation of a recklessly desperate population assumes naivety and is also without merit. The internet has made medical information universally and instantly available. The lay public is now informed. This is especially true for mothers of brain injured children who. as every caregiver is aware, leave no stone unturned in their quest for best outcomes for their children. (These mothers were the driving force for funding and performance of both McGill trials. Informed they are, recklessly desperate they are not.) Bad outcomes, fraud, and dishonesty are immediately exposed and the repercussions swift. Internet sites and special interest groups, e.g., the MUMS Network (Mothers United in Moral Support), a parent-to parent organization for parents of disabled children, have chat rooms and/or keep files on complaints and bad outcomes at treatment centers. There is no place to hide; the medical marketplace has become efficient. In addition, these parents compare LPHBOT to ALL forms of previous therapies. If LPHBOT had no effect on their children after the first round of treatment-parents would cease treatment. They would not throw good money after bad, travel great distances, inconvenience/disrupt their families, and expend significant amounts of time, energy, and resources for a worthless medical therapy. Instead, they go to great lengths to return for additional treatment or obtain the treatment in their home cities. They lobby their insurance companies, Medicaid officials, and legislators for economic and political relief, start hyperbaric companies or not-for profit treatment centers, and, in some cases, obtain training and install hyperbaric chambers in their homes. While these arguments are admittedly unscientific they form a powerful worldwide testimonial backdrop to the scientific points made above.
Conclusion
Evidence in both animal and human studies is accumulating for a positive effect of LPHBOT in chronic adult and pediatric neurological conditions. Understanding the drug definition of hyperbaric oxygen therapy and the principles of DNA oxygen signaling are the keys to appreciating the animal effects and understanding the human studies. Further studies in animals will reveal mechanisms while studies in adults and children will prove efficacy in different neurological conditions. However, no further studies need be done on HBOT in Cerebral Palsy. When the rules used to compose the Accepted Indications List are applied to Cerebral Palsy the evidence is found to exceed that of the majority of diagnoses on the list. It is time for responsible physicians to acknowledge this and add Cerebral Palsy to the list.
Paul G. Harch, MD is in private practice in New Orleans with Harch Hyperbarics, Inc. He is also Clinical Assistant Professor of Medicine and Director of the, Hyperbaric Medicine Fellowship, Department of Medicine, Section of Emergency and Hyperbaric Medicine, Louisiana State University School of Medicine, New Orleans, Louisiana. He can be contacted at www.hbot.com.
[Published in Exceptionsl Parent EP Magazine June 2004]


